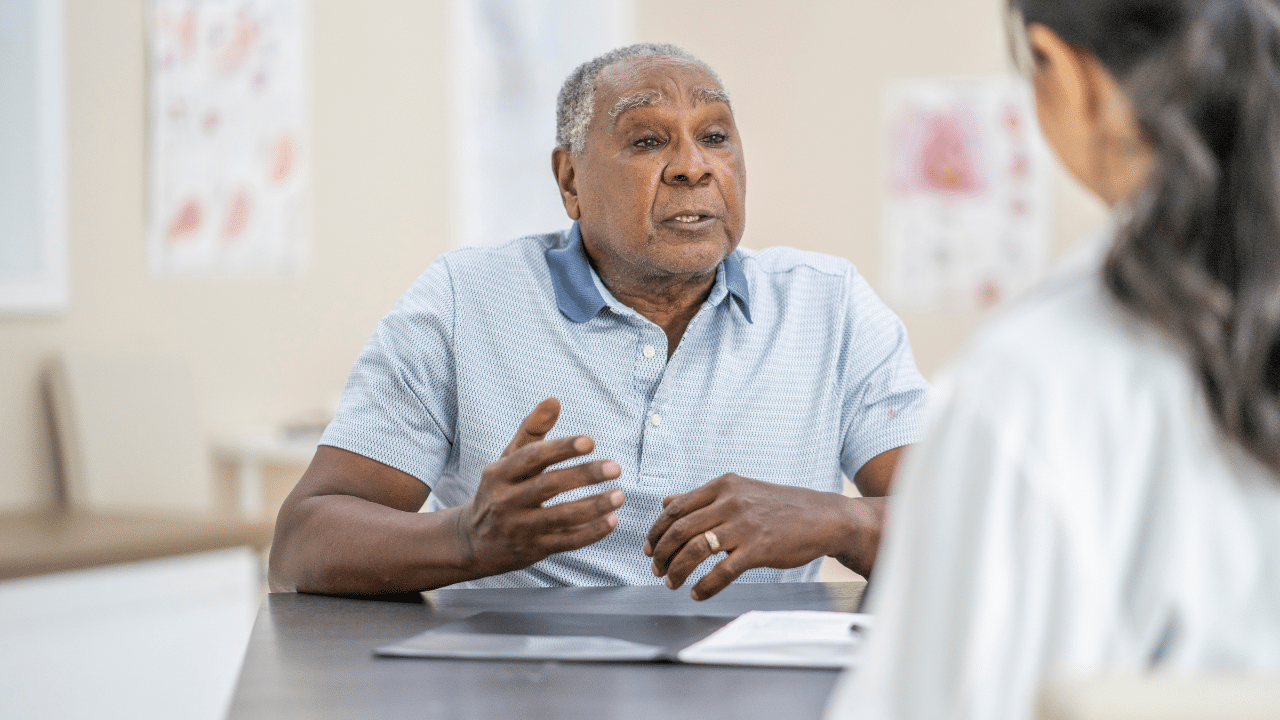
When we think about trauma, older adults are often not the first group that comes to mind. However, 70-90% of older adults have experienced a traumatic event in their lifetime, and they are particularly vulnerable to medical trauma.
Trauma-informed care is essential for supporting aging populations across healthcare, mental health, and social service settings.
Here’s What You’ll Learn in This Episode:
✅ The difference between trauma treatment and Trauma Informed Care
✅ The three E’s of trauma: Events, Experience, and Effects
✅ The impact of trauma across the lifespan, from adverse childhood experiences (ACEs) to end of life.
✅ The connection between PTSD, aging, and medical trauma
✅ The four R’s of trauma-informed care
✅ How culturally inclusive trauma-informed care improves outcomes for older adults and healthcare teams
Click here to Get your free Trauma-Informed Care Guide
How Does Trauma Affect Us Across the Lifespan?
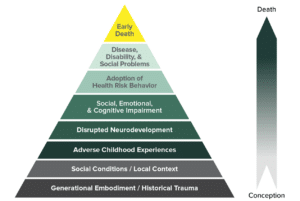
This is the graph from UCSF Center to Advance Trauma Informed Care demonstrating how Adverse Childhood Events influences health and longevity.
Key Takeaways:
What is Trauma-Informed Care?
Unlike trauma treatment, which provides direct medical and psychological care to directly address post-traumatic stress reactions, trauma-informed care is an approach that recognizes the impact of trauma and integrates that awareness into care settings. It ensures individuals feel safe, respected, and empowered in healthcare and social service environments.
Understanding Trauma in Older Adults
- Trauma is not just about single, catastrophic events—it can result from prolonged exposure to violence, discrimination, poverty, and even neglect.
- Many older adults have faced combat trauma, medical trauma, historical trauma, or community-based trauma.
- PTSD symptoms can emerge or worsen with aging due to role changes, health issues, and loss of coping mechanisms.
Post-Traumatic Growth in Older Adults
Not all trauma leads to long-term suffering. Many older adults experience post-traumatic growth, where they develop new strengths, deeper relationships, and a renewed sense of purpose.
The Four R’s of Trauma-Informed Care
- Realization – Understanding the widespread impact of trauma.
- Recognition – Identifying trauma-related signs and symptoms.
- Response – Implementing trauma-informed policies and practices.
- Resist Re-Traumatization – Ensuring care settings are safe and healing-centered
Why Trauma-Informed Care Matters in Aging Services
A trauma-informed approach:
✔️ Improves trust and engagement between older adults and providers
✔️ Leads to better health outcomes and reduces health inequities
✔️ Helps providers avoid burnout and fosters resilience within care teams
Want to become certified in Trauma-Informed Care for Older Adults? Check out Dr. Koepp’s six-hour certificate program.
Helpful Resources
- Trauma Informed Care with Older Adults Certificate Course (6 CEU credits)
- Article: Trauma and Older Adults: Acute Stress Disorder, PTSD, and Unique Considerations
- Trauma-Informed Care Guide for Older Adults: Download here
- Helping Older Adults After Disasters: A Guide by SAMHSA
- Helping Older Adults Prepare for Disasters: Essential Resources & Tips
- SAMHSA Disaster Distress Helpline: 1-800-985-5990
- National Crisis Hotline for Mental Health: Call 988 (Like 9-1-1 but for mental health emergencies)
References:
- Kaiser, A. P., Wachen, J. S., Potter, C., Moye, J., & Davison, E. (n.d.). Posttraumatic Stress Symptoms among Older Adults: A Review. National Center for PTSD. Retrieved March 24, 2024, from https://www.ptsd.va.gov/professional/treat/specific/symptoms_older_adults.asp
- Robertson M, Colburn J, Gerber M. Applying a trauma-informed approach to home visits. J Am Geriatr Soc. 2024; 72(5): 1322-1328. doi:10.1111/jgs.18743
- UCSF Center to Advance Trauma Informed Care. (2024, June 1). How trauma affects our health. Retrieved from https://cthc.ucsf.edu/why-trauma/
- Wu, X., Kaminga, A. C., Dai, W., Deng, J., Wang, Z., Pan, X., & Liu, A. (2019). The prevalence of moderate-to-high posttraumatic growth: A systematic review and meta-analysis. Journal of Affective Disorders, 243, 408–415. https://doi.org/10.1016/j.jad.2018.09.023